News
You only die once
Dying Matters Awareness Week will take place 12-18 May. This year's theme is #YODO - You Only Die Once.
Various events promoting openness about death, dying and bereavement will be taking place across the UK - see the Dying Matters website for more information. Several events are taking place in Scotland...
Good Life, Good Death, Good Grief, Faith in Older People and Edinburgh University Chaplaincy are working together to put on a Civic Café event. Already fully booked, the event will provide an opportunity to follow up the recent Malcolm Goldsmith Lecture given by Rabbi Baroness Neuberger on Dying well and why it matters.
A community-run You Only Die Once Death Cafe will take place in at 6.30pm in the Benarty Centre, Ballingry, Fife on 15th May. Free cake and a cuppa for participants - book in advance here: weblink.
The Aberdeen Gate Project will be taking a Before I Die wall to the Bon Accord Centre in Aberdeen on Saturday 17th May, 10am – 4pm. They will be engaging with the public and conducting a survey to gauge their thoughts, preparations and comfort around End of Life Issues.
Final Fling is joining in with a week long Take 5 campaign... encouraging you to take 5 minutes each day and do something to contribute to a good end. Check out the Final Fling website for more information.
NHS Fife is holding a free afternoon tea with death as the discussion. Thursday 15 May, Rothes Halls, Glenrothes, 2pm – 4pm. Attendance is free but numbers are limited so please book in advance.
Marie Curie Cancer Care are holding various events in Argyll & Bute throughout the week, all including refreshments, information from funeral directors, Age Scotland, Good Life, Good Death, Good Grief, solicitors, “record five wishes”, and an interactive Before I Die wall. 12th May –Dunoon; 15th May – Rothesay; 16th May – Lochgilphead. More information is available from Jennifer Layden.
NHS Tayside will be running an awareness and information event in Angus College on 15th May from 11am – 3pm. More information to follow.
Widowed and Young (WAY) are holding a Big Picnic on Sunday 18th May, in Pittencrieff Park, Dunfermline, from 12pm - 4pm. A nyone who would like to come along is invited. Meet on the grass in front of the museum, bring your own food. There will be entertainment for the children and more information is available on the WAY website.
A Before I Die wall will appear at Stobhill Ambulatory Care Hospital in Glasgow in Friday 16th May, from 10am - 1pm. NHS Greater Glasgow & Clyde staff will be on hand, engaging with the public surrounding dying matters and encouraging people to start to think about having conversations with loved ones - it is never too early to think about planning ahead.
Volunteers sought to participate in filming
 Do you have happy memories of someone who is now dead?
Do you have happy memories of someone who is now dead?
Has someone who has died played an important role in your life?
Would you be willing to share these memories in written form or within a short film?
This November, Good Life, Good Death, Good Grief will launch To Absent Friends: A Festival of Storytelling and Remembrance. The Scotland-wide festival will be an opportunity to remember ordinary people who have died but who live on in the memories and stories of the living. We are currently making a website and a short promotional film to advertise to absent friends and are seeking people to take part by sharing stories, memories and anecdotes on camera or in written form. Stories can be poignant or trivial, ordinary or exceptional, moving or humorous.
If you are interested, or would just like more information about what would be involved, please get in touch with Rebecca at Good Life, Good Death, Good Grief by Friday 4th April:
0131 229 0538 or rebecca@palliativecarescotland.org.uk
Facilitator available to run death, dying & bereavement workshops
 Organisations wishing to hold workshops to provide volunteers with practical education relating to death, dying and bereavement can now apply through good life, good death, good grief to access the services of an experienced facilitator, free of charge.
Organisations wishing to hold workshops to provide volunteers with practical education relating to death, dying and bereavement can now apply through good life, good death, good grief to access the services of an experienced facilitator, free of charge.
Background: who are these workshops designed for?
Living through difficult times relating to death, dying or bereavement is challenging and emotionally painful, and affects individuals, families and communities.
Throughout Scotland there are individuals who provide support to people in their community, for example church pastoral visitors and volunteer befrienders. Many people who volunteer for public sector or voluntary organisations have a role which includes dealing with practical or emotional effects of death, dying and bereavement.
Many individuals working in these roles may have the inclination or potential to take on more of a supportive role relating to death, dying and bereavement, but lack the confidence or skills to do so. These workshops are designed to provide participants with the opportunity to explore how they can better support the individuals and families they meet.
Workshop Facilitator
Joan Adam worked as a Macmillan Nurse Specialist and then a lecturer in palliative care for 20 years. She has a particular interest in helping people to help themselves and others in their organisation/community.Working withpeople in a small group can help develop knowledge, skills and confidence in talking about and supporting people through a range of issues related to planning for a good death, dying and bereavement.
Workshop details
Workshop 1: How do you talk about death? (2 hours)
This workshop aims to provide participants with the opportunity to explore and discuss:
- end of life issues, planning for the end of life and practical advice on how participants might better support individuals and families in their community
- the topics and issues which may arise during a discussion about death, dying and bereavement
- their own strengths and limitations
- how to access professional/social/voluntary support services
Workshop 1 can be run as a stand alone or with workshop two which would be held 4-6 weeks later.
Workshop 2: Facilitating small group discussions on end of life issues/ bereavement and loss (2 hours)
This workshop is aimed at anyone who wishes to hold discussions/run events relating to death, dying and bereavement within their own community, but would like some guidance on how to get started. The two half-day workshops will provide participants with the opportunity to explore:
- how to listen to and respond to issues out with their own comfort zone
- their experiences, skills, strengths, weaknesses and future learning needs relating to end of life issues within their organisation/ client group/ community
- how to plan and develop an initiative within their own community
There will be the opportunity to join a virtual peer support group following the workshop as participant develop their ideas and work towards completing and running their project/ initiative .
Participants who attend both workshops will be asked to undertake some preparatory work before attending the second workshop, to consider the type of initiative they would like to develop in relation to their work/organisation.
Applying to hold a workshop
To be eligible to apply to hold either/ both of these workshops, organisations must:
- Be (or become) a member of good life, good death, good grief (membership is free).
- Be able to provide a workshop venue in Edinburgh or the Lothians.
- Be providing the workshop for volunteers.
- Provide the workshop free of charge to participants.
- Take full responsibility for organising and holding the workshop, including:
- Provide an appropriate venue for the workshop/ training (including facilities: DVD, laptop and projector, flip chart, tea and coffee)
- Co-ordinate volunteer attendance at the training (minimum attendance:10/maximum attendance: 20)
- Take responsibility for the health & safety etc arrangements at the venue
- Provide reasonable travel expenses (public transport) from Edinburgh
To apply, contact: Rebecca.
Scottish Government staff mark Hospice Care Week
 On
Thursday 10th October, the Scottish Government offices at St Andrew’s House in Edinburgh were
visited by Before I Die – a
global public art project that invites people to reflect on their lives and
share their personal aspirations in public space.
On
Thursday 10th October, the Scottish Government offices at St Andrew’s House in Edinburgh were
visited by Before I Die – a
global public art project that invites people to reflect on their lives and
share their personal aspirations in public space.
Good Life, Good Death, Good Grief and the 100% Project brought the Before I Die walls to St Andrew’s House to mark Hospice Care Week 2013.
Before I Die was originally conceived by American artist Candy Chang, who explains on her website the inspiration behind the project: “After I lost someone I loved very much, I thought about death a lot. This helped clarify my life, the people I want to be with, and the things I want to do, but I struggled to maintain perspective. I wondered if other people felt the same way. So with help from old and new friends, I painted the side of an abandoned house in my neighborhood in New Orleans with chalkboard paint and stenciled it with a grid of the sentence ‘Before I die I want to _______.’ Anyone walking by could pick up a piece of chalk, reflect on their lives, and share their personal aspirations in public space.”
Rebecca Patterson, from Good Life, Good Death, Good Grief, said: “At Good Life, Good Death, Good Grief we believe that problems are caused in Scotland because as a society we are reluctant to be open about death, dying and bereavement. For example, people are unprepared for the experiences of death, dying and bereavement. Communities can be disempowered from providing support to people who are dying or bereaved. Health and social care professionals are unprepared for death-related discussions.
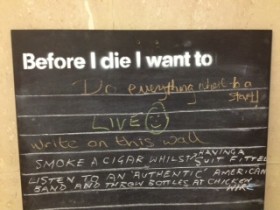 “We believe that many of these problems can be
solved by raising public awareness of ways we can all support each other
through the difficult times that come with death, dying and bereavement. Before
I Die walls are a meaningful and light-hearted way of bringing reflections
on life and death into public spaces.”
“We believe that many of these problems can be
solved by raising public awareness of ways we can all support each other
through the difficult times that come with death, dying and bereavement. Before
I Die walls are a meaningful and light-hearted way of bringing reflections
on life and death into public spaces.”
Hospice Care Week is held each year, as a week of celebration and action aimed at changing people's perceptions of hospice care, and to help raise the profile of hospice care across the UK.
Ali Kerr, Fundraising Manager at the Children’s Hospice Association Scotland added: ““CHAS understands that families who experience the death of a child experience isolation and stress through society’s reluctance to talk about death and dying. CHAS has a responsibility to play a part in helping to challenge these issues in the hope that this will make communication with and for families a little bit easier. That is why we set up the 100% Project, which aims to start conversations about death, dying and bereavement in a life-affirming way.”
So, what to St Andrew's House staff want to do before they die? Suggestions ranged from the practical “Before I die I want to retire” to the romantic “Before I die I want to find true love” to the whimsical “Before I die I want to smoke a cigar whilst having a suit fitted.”
MSPs recognise the need to be open about death
Seven MSPs voiced their support for more openness about death, dying and bereavement during a recent debate in the Scottish Parliament.
Nanette Milne MSP, whose parliamentary motion initiated the debate at Holyrood, said "the Scottish taboo around talking about death should be tackled". She also highlighted the importance of early identification, assessment and treatment of pain and the associated physical, psychosocial and spiritual problems, and the essential role palliative care plays in this.
 MSPs from across all parties agreed that openness is essential in
creating a society where people can discuss their needs and preferences for
care towards the end of their life.
Michael McMahon, MSP for Uddingston and Bellshill said: “I believe that Scottish society would benefit from being more
open to death, the dead and dying, and that we would become more aware of the
options and choices that are available when we are faced with the end of life.” Pictured (right) is Michael McMahon MSP taking part in Good Life, Good Death, Good Grief awareness week earlier this year, by writing on a Before I Die wall outside the Scottish Parliament.
MSPs from across all parties agreed that openness is essential in
creating a society where people can discuss their needs and preferences for
care towards the end of their life.
Michael McMahon, MSP for Uddingston and Bellshill said: “I believe that Scottish society would benefit from being more
open to death, the dead and dying, and that we would become more aware of the
options and choices that are available when we are faced with the end of life.” Pictured (right) is Michael McMahon MSP taking part in Good Life, Good Death, Good Grief awareness week earlier this year, by writing on a Before I Die wall outside the Scottish Parliament.
Neil Findlay, Lothian MSP, brought a personal note to the debate, reflecting on his experiences of the death of his father: “Scots are not very good at dealing with these types of things. Death is a time that brings out the best and worst in people. Often, we do not like dealing with all the practicalities surrounding death, expressing our emotions and taking time to look at the practical steps that we need to take. We do our best to avoid those things until we have to do them. We do not tell the people who are closest to us simple things such as how much we love them until it is too late.”
This debate was prompted by the publication of research which asked the question How good is primary care at identifying patients who need palliative care? Published in the European Journal of Palliative Care, the paper is the result of a study led by Prof. Scott Murray and Dr Lilin Zheng at the University of Edinburgh in collaboration with representatives from Marie Curie Cancer Care, and NHS Lothian.
The key findings of the study were that:
- Only 20% of patients with chronic heart, lung, liver or kidney conditions (organ failure) or dementia, either requested or were identified for palliative care before dying.
- 75% of cancer patients were identified for palliative care before dying.
- Most patients who were identified for palliative care received it too late to fully benefit – on average only 8 weeks before dying.
- GPs said that identifying patients for palliative care was fairly straightforward for those with cancer, who typically had a clear terminal phase.
- GPs generally found it difficult to discuss death and dying with patients, particularly with patients with a non-cancer diagnosis.
- Few patients openly discussed that they might die, thinking that this was a negative thing to do, although doctors thought it to be helpful for all concerned.
- Negative connotations associated with and a lack of understanding around terms such as ‘palliative’ and ‘hospice’ were also recognised as barriers for starting palliative care and support.
Reflecting on the research, Jim Hume, MSP for South Scotland emphasised the role of GPs: “One of the more enlightening areas of the research was the views of the health professionals. It is clear that GPs across Scotland are having real difficulty in identifying which non-cancer patients are appropriate for palliative care. They are also having difficulty in discussing death and dying with non-cancer patients with life-threatening conditions.”
Malcolm Chilsholm, Edinburgh Northern and Leith MSP drew attention to Good Life, Good Death, Good Grief, saying: “The good life, good death, good grief campaign highlighted in the
motion not only supports those going through the death and grieving process but
seeks to normalise that process and open up conversations on the surrounding
issues. Like the report, the campaign points out that it is never too early to
think about planning ahead for illness and death and that making plans when we
are healthy means that the pressure of making crucial decisions is lessened at
the point when sickness takes hold.”
Paisley MSP George Adam added his support for Good Life, Good Death, Good Grief, saying: “We need to ensure that more people know about that initiative so that,
when other families are in that type of position, they do not have to go
through the same difficulties.”
The Minister for Public Health, Michael Matheson MSP welcomed the research and reiterated the government’s recognition of the need for good palliative care to be provided in all care settings, on the basis of need rather than diagnosis. Recognising the need for openness about death, dying and bereavement, he said: "... none of the issues will be addressed quickly or easily. Individuals often have a natural aversion to talking about dying and death. Some good work has been undertaken, which members are aware of, through the good life, good death, good grief programme. We need to build further on that to allow those discussions to take place.”